Abstract
Background
FDG-PET-CT (PET), now considered the standard of care for remission assessment in FDG-avid lymphoma has high predictive value for survival outcomes. However, about 20% of PET negative patients will relapse, while only 30-40% of PET positive patients can be rescued with salvage treatments. Aim of the research is to evaluate if combining absolute monocyte count (AMC) at staging, a prognostic factor related to lymphoma microenvironment with end of treatment PET (EOT-PET) results can increase the already strong predictive value of PET.
Patients and Method
The study analyzed patients diagnosed with Diffuse Large B-Cell Lymphoma recorded at Modena Cancer Center, S. Andrea Hospital of Rome and B- Bnai Zion Medical Center of Haifa from 2007-2015, and treated with R-CHOP or CHOP-like regimens. Eligibility criteria were: availability of clinical characteristics, blood differential, basal and end of treatment CT (BAS-CT and EOT-CT), PET scan (BAS-PET and EOT-PET), and survival outcomes. Response evaluation was based on 2007 Cheson criteria. The PET results were revised using Deauville criteria; AMC at diagnosis > 630/mmc were considered predictive of poor prognosis. Progression free survival (PFS) was defined as the time from study entry to the time of any documented progressive disease (PD) or death from any cause; failure free survival (FFS) was defined as the time from study entry to the time of any documented lack of complete response (CR), relapse after CR or death from any cause. PFS and FFS were assessed by Kaplan-Meier estimates and compared to risk groups using the log-rank (LR) test.
Results
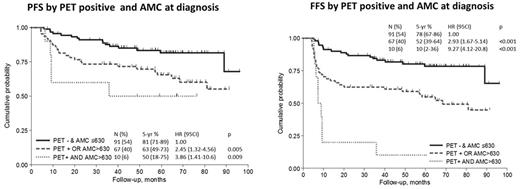
The study included 186 patients: the median age was 60 years; 62% were in stages III-IV and 33% had an International Prognostic Index (IPI) score 3-5. At EOT-CT evaluation, 146 patients (79%) reached a complete response and 38 (21%) achieved PR, SD or progressed during treatment. At EOT-PET analysis 29 patients (17%) had Deauville score ≥4 and were considered PET positive. After a median follow-up of 64 months (range: 7-119 months) 5-years PFS and FFS was 72% and 64%, respectively. By EOT-PET the 5-years PFS was 80% for negative and 44% for positive patients (p<0.001). There was no statistically significant difference in PFS by AMC, while it was prognostic in FFS (p=0.019). Given the prognostic value of both EOT-PET and AMC, we stratified patients into 3 groups: the low risk level (negative EOT-PET and AMC ≤630/mmc/L) had a 5-years PFS of 81% (95% CI: 71-89%) and a 5 years FFS of 78%(95%CI:65-86), the intermediate level (EOT-PET positive or AMC > 630/mmc/L) had a 5-years PFS of 63% (95% CI: 49-73%) and a 5 years FFS of 52%(95%CI:39-64), and the high risk level (EOT-PET positive and AMC > 630/mmc/L) had a 5-years PFS of 50% (95% CI: 18-75%) and a 5 years FFS of 10%(95%CI:2-36), respectively. (Fig 1 a.b).
Conclusion.
Although retrospective, our study shows that combining EOT-PET results evaluated with Deauville criteria with the AMC at diagnosis we are able to discriminate groups of patients with low, intermediate and high risk. We hypothesize that EOT-PET and AMC at diagnosis are the expression of two aspects of the disease; positive PET reflecting the persistence of the lymphoma, and the elevated AMC in the peripheral blood as a biomarker of the tumor microenvironment/cytokines. Based on this hypothesis and on the strong prognostic value of both parameters, we are planning to validate our model in a larger and independent cohort of patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.